EVENT PROGRAM
SCHEDULE-AT-A-GLANCE
Join us for an enriching symposium tailored for healthcare professionals, focusing on the nuances of nursing transition and well-being. Dive deep into concurrent sessions addressing challenges in the Emergency Department, the significance of well-being in nursing, and the power of independent practice. Explore TTP Power sessions that shed light on leadership, preceptorship, and communication strategies. Engage in Learner Focused Seminars that emphasize diversity, equity, inclusion, and the ANA Code of Ethics. The event culminates with a general session on mastering precepting, ensuring the success of future nurses. Don't miss this comprehensive exploration of nursing's evolving landscape.
PreCons
Sunday, April 28
-
8:00 a.m. – 5:00 p.m.
APPFA Workshop
-
8:00 a.m. – 5:00 p.m.
ANCC PTAP Workshop
DAY 1
Monday, April 29
-
9:00 a.m. – 6:00 p.m
Registration Open
-
9:00 a.m. – 10:30 a.m.
ANCC PTAP and APPFA Program Director Meeting (invite only)
-
11:00 a.m. – noon
ANCC PTAP and APPFA Appraiser Appreciation Meeting (invite only)
-
11:00 a.m. – 1:00 p.m.
Sponsor Tables Open
-
1:00 p.m. – 2:30 p.m.
Opening General Session –
No CE offered -
2:45 p.m. – 3:45 p.m.
Concurrent Sessions - 1
-
4:00 p.m. – 5:00 p.m.
Concurrent Sessions - 2
-
5:00 p.m. – 6:30 p.m.
Welcome Reception
DAY 2
Tuesday, April 30
-
8:00 a.m. – 4:30 p.m.
Registration Open
-
7:30 a.m. – 8:30 a.m.
Continental Breakfast
Sponsor Tables Open -
8:30 a.m.– 9:30 a.m.
Concurrent Sessions - 3
-
9:45 a.m.– 10:45 a.m.
Concurrent Sessions - 4
-
11:00 a.m. – noon
Concurrent Sessions - 5
-
Noon – 1:00 p.m.
Lunch
Sponsor Tables Open -
12:45 p.m.– 1:45 p.m.
Posters Presenters Available
-
1:45 p.m. – 3:00 p.m.
General Session and PTAP Celebration –
No CNE offered -
3:15 p.m.– 4:15 p.m.
Concurrent Sessions - 6
-
4:30 p.m.– 5:30 p.m.
Concurrent Sessions - 7 –
sponsored sessions –
No CNE offered
DAY 3
Wednesday, May 1
-
7:30 a.m.– 8:30 a.m.
Continental Breakfast
Poster Viewing -
8:30 a.m.– 9:30 a.m.
Concurrent Sessions - 8
-
9:45 a.m.– 10:45 a.m.
Concurrent Sessions - 9
-
10:45 a.m.– 11:15 a.m.
Snack Break with Posters
-
11:15 a.m. – 12:30 p.m.
Closing General Session –
No CNE offered

Advanced Practice Provider Fellowship Accreditation™ (APPFA) Workshop
Sunday, April 28 | 8:00 a.m. – 5:00 p.m.
Attend this one-day, in-person workshop to learn about the 2023 APPFA Manual accreditation process.
Immerse yourself in the APPFA standards and learn how to apply them in your practice setting. Get an insightful overview of the accreditation process before collaborating in small groups to review ideas, share experiences, and get feedback on practice exercises.
This workshop is highly recommended for potential new applicants, applicants, and reaccrediting programs. It provides an overview of the APPFA eligibility, standards, application, and review processes, and awarding of accreditation.
The 2023 APPFA Manual is applicable to any applicant interested in a cycle starting in 2023.
Learn more about APPFA: Advanced Practice Provider Fellowships Accreditation (nursingworld.org)
Who Should Attend:
- APP Program Directors
- APP Leaders
- APRN and PA Leaders
APRN participants successfully completing this activity will be awarded 8.75 contact hours.
This activity has been reviewed by the AAPA Review Panel and is compliant with AAPA CME criteria. This program is not yet approved for CME credit. Conference organizers plan to apply for up to 10 AAPA Category 1 CME credits from the AAPA Review Panel. The total number of approved credits is yet to be determined.
8:00 a.m.– 5:00 p.m. ET
Workshop Agenda
- Welcome
- Conceptual Model and Eligibility Criteria
- Writing Tips
- Criteria Overview - Program Leadership
- Criteria Overview - Program Goals and Outcome Measures
- Criteria Overview - Organizational Enculturation
- Criteria Overview - Development and Design
- Criteria Overview - Practice-Based Learning
- Criteria Overview - Accreditation with Distinction (AWD)
- Activities (throughout the day)
- Application and Review Process
- Next Steps and Closing

ANCC Practice Transition Accreditation Program® Workshop
Sunday, April 28 | 8:00 a.m. – 5:00 p.m.
ANCC’s Practice Transition Accreditation Program® (PTAP) is the global standard for transition to practice programs.
Attend this one-day, in-person workshop to learn about the ANCC 2024 PTAP Manual accreditation process.
Immerse yourself in ANCC’s PTAP standards and learn how to apply them in your practice setting. Get an insightful overview of the accreditation process before collaborating in small groups to review ideas, share experiences, and get feedback on practice exercises.
This workshop is highly recommended for potential new applicants, new applicants, and reaccrediting programs. It provides an overview of the ANCC PTAP eligibility, standards, application and review processes, and awarding of accreditation.
The 2024 PTAP Manual is applicable to any applicant interested in a cycle starting in 2024.
Learn more about PTAP: Practice Transition Accreditation Program | ANCC | ANA (nursingworld.org)
Who Should Attend:
- Nurse Residency Program Directors
- NPD Practitioners
Participants successfully completing this activity will be awarded 8.75 contact hours.
8:00 a.m.– 5:00 p.m. ET
Workshop Agenda
- Welcome
- Conceptual Model and Eligibility Criteria
- Writing Tips
- Criteria Overview - Program Leadership
- Criteria Overview - Program Goals and Outcome Measures
- Criteria Overview - Organizational Enculturation
- Criteria Overview - Development and Design
- Criteria Overview - Practice-Based Learning
- Criteria Overview - Accreditation with Distinction (AWD)
- Activities (throughout the day)
- Application and Review Process
- Next Steps and Closing
9:00 a.m. – 6:00 p.m.
Registration
9:00 a.m. – 10:30 a.m.
Program Director Meeting (separate registration required)
Network with your other ANCC PTAP and APPFA program directors. Hear from the ANCC PTAP/APPFA team!
Connect with your colleagues during this first in-person ANCC PTAP/APPFA Program Director meeting.
-
- Celebrate successes
- Troubleshoot questions
- Take part in tabletop exercises
11:00 a.m. – noon
Appraiser Appreciation Meeting (separate registration required)
Network with fellow ANCC PTAP and APPFA appraisers.
Celebrate your successes!
Learn about future plans for PTAP and APPFA.
11:00 a.m. – 1:00 p.m.
Sponsors Tables and Snack
1:00 p.m. – 2:30 p.m.
General Session; GS-01
Opening Remarks
Diversity, Equity, and Inclusion: How We Advance Health Equity for Our Patients and Workforce
Dr. Scharmaine Lawson, DNP, FNP, PMHNP, FAANP, FAAN
What does it take to actually advance health equity for patients and the nursing workforce? This presentation offers a first-hand account of how one entrepreneur has developed an innovative program that has helped to foster trust between the nursing community and neighborhood schools.
2:30 p.m. – 2:45 p.m.
Break
Dr. Scharmaine Lawson book signing
2:45 p.m.– 3:45 p.m.
Concurrent Session 1; CS-01
TTP Pitch – Organizational Enculturation — CS-01-A
Keeping Them Safe: Empowering Nurse Residents with De-Escalation Strategies
Rosa Rousseau
Workplace violence continues to impact the nursing workforce, and prevention is crucial to keep new nurses safe. This presentation shares how one nurse residency program integrated verbal de-escalation strategies and virtual simulation scenarios to provide nurses with tools to manage and prevent aggressive behaviors.
Engaging New Graduate Nurses in Magnet® Collaborative Council Meetings
Marsha Deckman, MSN, RN, NE-BC and Patricia Alban, MSN, RN, CEN, PCCN, NPD-BC
New graduate nurse (NGN) participation in the Magnet® Collaborative Council Day is part of organizational enculturation. This best practice engages NGNs to better understand council structure and participate in the organization’s strategic goals.
Real Talk Sessions: An Essential Mental Health Component of an RN Residency
Kayce K Tugg, MSN, RN, AOCN and Kelly Delgado, MSN, RN-BC
This session focuses on how the mental health needs of RN residents can be met through an innovative residency-supportive component entitled Real Talk Sessions (RTS). Presenters share the processes involved in RTS development and administration as well as RTS effects on RN residents.
TTP Power – Preceptors — CS-01-I
Standardizing Preceptor Selection Utilizing a Valid Tool
Crystal Davis, MSN, RN, NPD-BC, PHN
How are preceptors selected? This session explores the process change undergone to ensure all preceptor candidates are selected utilizing a valid tool that addresses appropriate competencies. Presenters discuss scalability to meet current and future preceptor training demands.
From Resident to SuperNurse: Unlocking New Graduate Precepting Powers
Angela Lochridge, MSN, RN, NPD-BC and Lauren Thorngate, PhD, RN, CCRN-K
In this current climate of staffing constraints, one organization has developed an innovative curriculum addition that prepares residents to be preceptors and promotes early professional development. Residents build leadership skills and the organization benefits with the expansion of its preceptor pool.
Learner Focused Seminar – Games-Based Learning — CS-01-K
Are You Game? How Game-Based Learning Can Improve Learning and Engagement
Caitlyn Hall, BSN, RN, CPN and Kristi Myers, MSN, RN, CPN
This presentation discusses and takes participants through a game-based learning strategy to engage and improve learning among nurse residents and engagement among nurse preceptors in the practice-based setting.
TTP Solution – Well-being APP Fellowships — CS-01-M
Early Career Introduction to APP Well-being Tools Leads to Increased Provider Satisfaction and Retention
Lori Vasquez, DMS, PA-C and Barb Winningham, DNP, CNM, WHNP-BC, FACNM
This organization’s APP fellowship program believes that providing new APPs with well-being tools is crucial for provider satisfaction, improves patient outcomes, and promotes employee retention. Presenters share how they integrated multiple well-being tools into the program, including invitation of all APP fellows to a free, annual APP well-being retreat.
Integration of a Clinical Psychologist to Ensure Mental and Emotional Stability of Fellows
Courtney Coker, MSN, RN, AGACNP-BC and Nicole Gorecki, DNP, APRN, AGACNP-BC, CCRN
The inclusion of a clinical psychologist into this organization’s transition to practice program has proven to be an integral part of ensuring the emotional stability of fellows in a high-stress, high-acuity work environment.
Working in Wellness: Supporting Learner Well-being Throughout a Transition to Practice Program
Patricia Pease, MSN, FNP-BC and Tonya Ureda, MS, FNP-BC
Connecting learners with available wellness resources is a vital part of the support offered by preceptors, mentors, and program leadership. Describing a variety of methods to address learner well-being through this presentation encourages others to consider implementation within their programs.
Resident/Fellow Showcase: APP Fellows EBP/QI/Research Projects — CS-01-L
Use of Pasteurized Human Donor Breast Milk to Decrease Formula Supplementation in Newborn Nursery Setting
Nicole Fazio, DNP
This presentation reviews the well-known benefits of breast milk and explains how this QI initiative strives to increase exclusive breastfeeding rates by offering pasteurized human donor breast milk as an alternative to formula supplementation in a newborn nursery setting.
The Write Way: An Innovative Process Improvement Project to Enhance the Quality of Progress Notes
Hanz De Leon, MSN, ACNPC-AG
This quality improvement project standardized progress notes utilizing novel templates and comprehensive note-writing guides aimed to increase quality scores evaluated with a modified validated tool. Outcomes revealed a noteworthy 40% combined average increase in note quality and a decrease of 25% time spent in note writing.
When to Extend? A Surveillance Protocol for Stage 1 Kidney Cancer Patients
Jade Robinson, MSN, MPH, RN, AGACNP- BC
No current guidelines exist for identifying young patients with stage 1 kidney cancer at high risk for recurrence in which surveillance should be extended greater than five years. A clinical pathway was created that identifies 10 clinical criteria characterized as high risk for recurrence that warrants extended surveillance.
3:45 p.m.– 4:00 p.m.
Break
4:00 p.m. – 5:00 p.m.
Concurrent Session 2; CS-02
TTP Power – Sustainability — CS-02-A
Herding Kittens: Ensuring Ongoing PTAP Alignment and CMS Eligibility in Multi-Site RN Residency Program
LeAnn Ogilvie, MSN, MHA, RN
Ensuring ongoing PTAP alignment in a large, multi-site, multi-specialty RN residency program can be challenging. Seeking annual Center for Medicare and Medicaid Services (CMS) reimbursement for an eligible program requires consistent monitoring to ensure alignment. Attendees benefit from proven tools and developed strategies to sustain a consistent, quality program.
Let's Retreat: Building Engagement and Inspiring Greatness
Alaina Tellson, PhD, RN, CLNC, NPD-BC, NE-BC
A large organization shares how it uses retreats to build engagement in its program team and inspire others to greatness. This presentation shares the benefits and outlines of a successful retreat that leads to improving a program through feedback and buy-in.
TTP Solution – Program Goals and Outcome Measures — CS-02-I
Nurse Residency Program Increases the Number, Quality, and Retention of New Graduate Registered Nurses
Keith Hoshal, MSN, RN, NPD-BC, OCN and Janette V. Moreno, DNP, RN, NEA-BC, NPD-BC
This session explores how leveraging collaborative academic partnerships and utilizing a selection tool for the clinical placement of senior prelicensure nursing students can increase the number, quality, and retention of new graduate registered nurses hired into a nurse residency program.
The Implementation of Gratitude Practices and Perceived Stress among New Graduate Nurses
Jessica Paine, MSN, RN, CMSRN, NPD-BC and Kimi Clark, MSN, NPD-BC, CCRN
This session describes an intervention used to determine the impact of perceived stress among new graduate nurses in a TTP program. The intervention was a synchronous presentation accompanied by a PowerPoint, which described the practice of gratitude and potential benefits of these practices.
Increasing Retention, a Healthy Workforce, and Hospital ROI: A Novel Approach to TTP
Jamie M. Emery, MSN, RN, NPD-BC, CEN, CFRN and Lois Yearous, MSN, RN, NPD-BC
Amid global staffing challenges, this 12-hospital system led a longitudinal study on a comprehensive nurse residency program that begins with recruiting nurse techs and empowers new grads during the critical 7-12 months of residency. The novel approach yielded 90% retention, 22.8% turnover reduction, and $8.7 million in annual savings.
Learner Focused Seminar – Trauma Informed Care — CS-02-K
Trauma-Informed Care Techniques for Real-World Verbal De-Escalation
Johnny Woodard, MSN, RN, PMH-BC and Tessa Hensley, MSN, RN, NPD-BC
Practical tools and techniques for verbal de-escalation can be implemented immediately in any practice setting. This session explores de-escalation through the lens of trauma-informed care as well as the impact it has on health care. Participants will discuss and practice steps to mitigate escalation.
TTP Power – APP Fellowships – Curriculum — CS-02-M
Curriculum Development for Transition to Practice Programs
Julie Durand, DNP, MBA, APRN, PMHNP-BC
This presentation details the recommended steps in developing a robust curriculum for learners of any type. Practical steps are described to assist programs in mapping the curriculum based on a national standard, site-specific competencies, and identified cohort and individual knowledge deficits.
Fellowship Fridays: When Learner Feedback Drives the Evolution of the Program
Whitney Lerch, PA-C and Kathryn Williams
Presenters describe development and implementation of "Fellowship Fridays," a core curriculum component integrated into an existing large, multi-track pediatric APP fellowship program. Designed in response to APP fellow feedback, this new curriculum strengthens the program's alignment with multiple APPFA practice-based learning standards.
Resident/Fellow Showcase: RN Resident EBP/QI/Research Projects — CS-02-L
New Graduate Nurse Shift Checklist
Chioma Oghenekome, BSN, RN and Diane Pierre, BSN, RN
This session shares the development and utilization of a new graduate nurse resident standardized shift checklist to guide critical thinking and organizational competence during orientation and beyond.
Working Smart with Smartsheet and Redcap: Optimizing Prep Work for RN Residency Program Workshops
Jennifer Marie Gidaya, BSN, RN-BC
Due to the new graduate residency program workshop preparation being extensive, resource-intensive, and costly, this program sought to find different avenues to decrease resource utilization and cost. This led to the utilization of digital cloud-based platforms for workshop preparation.
Health Care Inclusivity: Providing Quality Communication to Limited English-Speaking Pediatric Patients and Families
Tylan Murphy, BSN, RN and Brie Williams, BSN, RN
Language barriers in the perioperative setting decrease quality of health care. This session describes the use of a smartphone application as well as the addition of Spanish phrases that operating room staff use to send intra-operative text updates to patients and their families.
5:00 p.m. – 6:30 p.m.
Reception
7:30 a.m. – 4:00 p.m.
Registration & Info Booth
7:30 a.m. – 8:30 a.m.
Breakfast and Sponsorship Tables
8:30 a.m. – 9:30 a.m.
Concurrent Session 3; CS-03
TTP Solution – Organizational Enculturation — CS-03-A
Health Literacy and Cultural Competence Awareness for the Nurse Resident
Marina Grennen and Patricia Alban, MSN, RN, CEN, PCCN, NPD-BC
This session explores the impact of NPD practitioners on promoting inclusion and providing education on unconscious bias and health disparities promoting individualized nursing care to self-awareness in their professional practice.
Acute Care Academy: Transitioning with Confidence
Carrie Kronberg, MNE, RN, CCRN-K, NPD-BC and Tyler Niesen, MSN, RN, CCRN-K
Acute Care Academy is an ongoing, two-tiered program that provides onboarding support through experiential learning in three classes and leader check-ins. The ongoing tier of the program includes support through clinical mini meetings, skill simulations and nurse pathway resources for further professional development.
Expectations Versus Reality: How to Navigate OE3 with Fun, Flair, and Level-Setting
Tessa Hensley, MSN, RN, NPD-BC, CDCES, CPN and Megan Unfried, MSN, RN, NPD-BC
This session reviews and defines OE3 while exploring the set-up, implementation, and follow-up from activities shared in their transition to practice program. These strategies have been honed over the last six years and have proved to be a best practice.
TTP Power – Goals and Dashboards Oh My! — CS-03-I
Going for the Goal!
Michelle Yeatts, MSN, RN, CEN, NPD-BC and Kristina Boyer, MSN, RN, CNOR, NPD-BC
Presenters share how to align strategic hospital goals with PTAP goals and practical ways to keep goal progress at the forefront of the program.
Seize the Data! The PIVOTal Role of Internal Dashboards for a System Nurse Residency Progra
Stephanie DeMaio, MSN, RN, NPD-BC, CMSRN
Nurse leaders looking to ensure an impactful transition to practice program are invited to discover the transformative power of seizing the data. This presentation shows how dashboards play a pivotal role in transforming data into actionable insights and ensuring data-driven decisions and quality in transition to practice programs.
Learner Focus Seminar – Peer-to-Peer Support — CS-03-K
Removing the Masquerade Mask: Increasing Peer-to-Peer and Reflection Time
Denise R. Norton, MSN, RN, NPD-BC, PCCN and Shelly D. Reeve, MSN, RN, PCCN
The Nurse Residency Program recognized the need for more peer-to-peer and reflection time to support the learners in identifying how similar their feelings are as newly licensed nurses.
TTP Solution – APP Fellowship – Simulation — CS-03-M
Embedding a Simulation Curriculum into an APP Fellowship
Lisa Pierce, DNP, APRN, CPNP-AC and Meghan Weber, DNP, MBA, APRN, FNP-BC
This presentation describes how one organization successfully embedded a comprehensive simulation curriculum, including case scenarios, procedures, and virtual reality, into a large APP fellowship program with both inpatient and outpatient specialties.
A Modified Queen’s Simulation Assessment Tool to Evaluate Competence in APP Fellowships
Olivia Nicastro, ACNP-BC
Presenters share a modified Queen's Simulation Assessment Tool as an objective way to evaluate competence of APP Fellows. This tool would be the first valid and reliable tool to evaluate competence within simulation for APP fellowships.
Enhancing Advanced Practice Provider Fellowship Education through Simulation
Joanna Tomicich, MSN, RN, NP-C and Al-Zada Aguilar, DNP, ACNP-BC
Presenters share how integrating simulation-based learning can enhance advanced practice provider learner development.
Resident/Fellow Showcase: APP Fellows EBP/QI/Research Projects — CS-03-L
Art and Clinical Assessment: Incorporating Visual Thinking Strategies into APP Education
Elena Abascal, DNP, PMHNP-BC
This session teaches participants about an evidence-based educational tool that uses art analysis to enhance clinical assessment skills. Presenters discuss a QI project in which participants were taught Visual Thinking Strategies (VTS), an extensively studied framework for implementing art analysis into clinical education.
Age-Friendly Health System: Improving Care of Older Adults in Ambulatory Practices Using the 4Ms
Huiqian Han, DNP, RN, AGPCNP-BC
This presentation explores the implementation of the 4Ms framework in the ambulatory care setting, focusing on improving care for older adults in ambulatory settings, with a particular emphasis on the impact on health care providers' confidence and proficiency.
Blood Stream Infections in ECMO Patients Relative to Cannulation
Christopher Ray and Will Westmoreland
This session features an examination of blood stream infection rates in ECMO patients relative to anatomical and/or hospital location of cannula placement.
9:30 a.m. – 9:45 a.m.
Break
9:45 a.m.– 10:45 a.m.
Concurrent Session 4; CS-04
TTP Power – Systems — CS-04-A
Centralized Nurse Residency Model: A Layered Leadership Approach to Support New Graduate Nurses
Tracey Whitley, MSN, RN, NPD-BC
A centralized, rotational nurse residency can succeed in a large hospital system. Program directors serve as direct-line leaders for all residents who enter the organization in their first year of practice. A centralized leadership model allows for additional support at the resident, unit, facility, and system levels.
Ensuring Standardization Accreditation Standards for Mega Sites: Navigating Alignment Pathways
Michelle Scortzaru, MNS, RN, NPD-BC and LeAnn Ogilvie, MSN, MHA, RN
Ensuring and sustaining standardization is a crucial responsibility for mega-site programs. Therefore, a thorough strategy encompassing site selection, continuous alignment, and persistent enhancement is imperative to cultivate excellence and uphold alignment standards. This presentation elucidates the process employed by an accredited mega-site to ensure initial and ongoing program alignment.
TTP Solution – Curriculum — CS-04-I
Enhancing the Integration of Evidence-Based Practice for Newly graduated Nurses in a Cancer Center
Majeda AL-Ruzzieh, PhD, RN and Yahia Moh'd AL-Helih
The transformative path intended to improve EBP for nurses working in a cancer center is described in this presentation. It demonstrates the coordinated efforts made by the nursing department to improve patient outcomes and standards of care.
Diversity and Inclusion Training for Residents
Jake White
A Diversity and Inclusion Training Program was created and implemented in 2023 for residents within the organization.
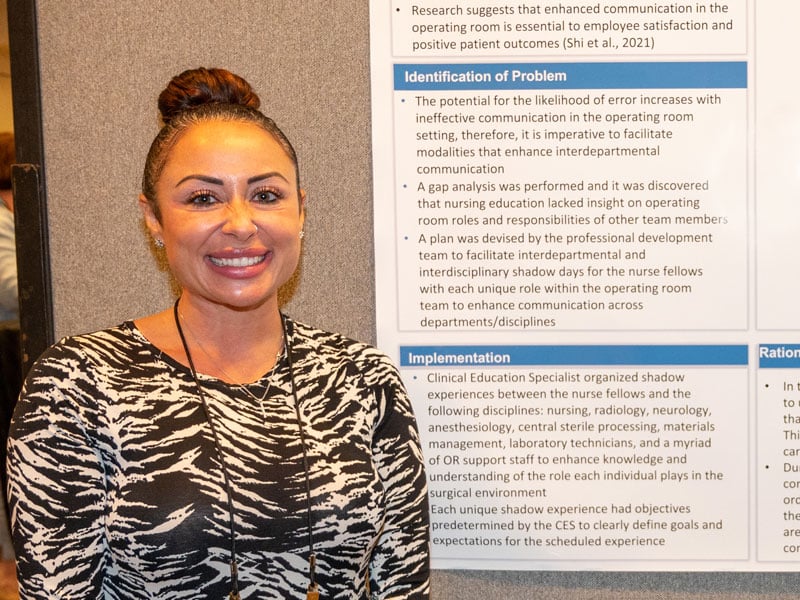
Charge Nurse Workshop
Melanie Marco, MSN, APRN, AGCNS-BC, NPD -BC and Stephanie Marrotte, RN, BSN-BC
Presented by a program director and nurse manager, this session features case studies, question and answer sessions, group work, reflection, and gamification.
Learner-Focused Seminar – Presentation Skills — CS-04-K
Foundational Skills for Professional Presentations
Tonya Ureda, MS, RN, FNP-BC, NE-BC and Suzette Stone, PhD, MSN, Mdiv, RN, PPCNP-BC, NEA-BC
This seminar will equip learners with an introduction to professional presentation skills. The goal is to encourage learners to submit scholarly work for presentations in the future as they expand their careers as APPs.
TTP Solution – APP Fellowship – Leadership — CS-04-M
A Program Letter of Agreement in APP Fellowship for Hospital Systems
Olivia Nicastro, ACNP-BC and Joanna Tomicich, MSN, RN, NP-C
Presentation of a template to build a program letter of agreement for APP fellowship programs that incorporate learning rotations at sister sites within large health systems.
The Implementation of an APN Fellowship Program to Improve Retention and RN-to-APN Transition
Jodi Galesi
This study investigates if an APN fellowship program could improve RN-to-APN retention in a large, academic medical center and improve the perceived experience of role transition for RN to APN.
Fine-Tuning the Process: Optimizing Recruitment and Onboarding Strategies for APP Fellowships
Meghan Weber, DNP, MBA, APRN, FNP-C and Lisa Pierce, DNP, APRN, CPNP-C
One APP fellowship program recognized an opportunity to evaluate and optimize the recruiting and onboarding process for APP fellows. The leadership team successfully implemented multiple strategies to increase recruitment locally and nationally and alleviated barriers to credentialing, resulting in a streamlined process from application to orientation.
Resident/Fellow Showcase: RN Resident EBP/QI/Research Projects — CS-04-L
Why Can't You Just P.A.U.S.E?
Ashley Carothers, RN and Brandi Jo Epperson, RN
This session highlights the implementation of P.A.U.S.E: Pause, Acknowledge, Unpack, Support, Evaluate – a formal debriefing process for staff who experience a traumatic event. The goal is to ensure support for those involved, giving them time to reflect and process to help mitigate moral injury that can lead to compassion fatigue.
Nurse-Led Vital Signs in the Acute Care Setting
Megan Chiglo, BSN, RN and Maya Maldonado, BSN, RN
This project identified cost-efficient methods that could be implemented in the RN workflow to increase patient interactions and promote more engagement in health-related dialogue. This presentation focuses on nurse- to-patient relationships to increase face-to-face engagement and collaboration leading to higher patient satisfaction scores.
From Scrubs to Snuggles: How Therapy Dogs Support New RNs
Alison Kovach, MSN, RN, CNL and Amy Bahena, RN
In this nurse residency program, over the course of one month, participating seminars received animal-assisted therapy sessions roughly 30 minutes in duration. These sessions were designed to help alleviate the stress and/or anxiety burden of new nurses' transition to practice. Impacts were surveyed in a pre-post intervention format.
10:45 a.m.– 11:00 a.m.
Break
11:00 a.m. – noon
Concurrent Session 5; CS-05
TTP Power – APP Fellowship – Professional Development — CS-05-A
Advancing Competency: The Leadership Journey from Clinical Coordinator to Specialty Leader
Aaron Lamale, MS, RN, FNP, AGACNP-BC and Kelly Bugos, MS, RN, ANP-BC, NPD-BC, AOCNP
A clinical coordinator role is essential to the structure, function, growth, and success of an APP fellowship program. Formal role progression and competency evaluations lead to role clarity and retention. Best practice competency evaluations provide visibility to operational leaders and can be implemented in any transition to practice program.
An Education Series to Promote the Clinical and Professional Development of the Advanced Practice Provider
Tonya Ureda, MS, RN, FNP-BC, NE-BC and Patti Pease
This session shares one strategy for enhancing the education of fellows through a didactic education series. The presentation is geared toward program directors and faculty members.
TTP Power – Well-being (APP and RN Fellowship) — CS-05-I
Cultivating Fellow Well-being with Teaching, Tools, and Team Coaching
Leann Li, MSN, RN, CMCN, NC-BC and Cynthia Allison, MSN, PMGT-BC
The seeds of wellness are planted early and carefully nurtured as fellows grow throughout the program. The Individual Health and Wellness Assessment (IHWA) and My Self Care Plan support well-being evaluation via personal introspection for individualized goal setting and attainment. In one case, it may have even saved a life!
Elevating Wellness: Deployment of a Comprehensive Mental Well-being Program in an APP Fellowship
Brad Stoecker, MD and Lisa Pierce, APN
The presentation engages with leaders of other programs to describe how an APP fellowship program uses a multiphase approach to address fellow wellness.
TTP Power – Credentials and Certifications — CS-05-K
Those Credentials Look Great on You! Get Fitted for Your Certification Journey.
Marianne Horahan, MBA, MPH, RN, CPHQ, NEA-BC, CAE
What does it mean to have certification credentials after your name? What are the steps to earning and maintaining certification? The speaker will share the value of certification and how to individually tailor the certification journey.
Types of individual credentials: Competitors or complements
Tara Myers, Ph.D., ICE-CCP
This session will focus on differences between types of individual credentialing, such as certification, micro-credentials, and assessment-based certificates. ANCC will discuss development, use, pros and cons, and stakeholder perspectives of the options. There will also be time for audience questions and discussion.
TTP Solution – APP Fellowships – Creative Solutions — CS-05-M
Private Physician Practices’ Role in Development of an APP Fellowship
Maren Wiseheart, APRN, CCNS, ACNP and Courtney Coker, APRN, AGACNP
Private physician practices have a wealth of knowledge to construct and maintain an APP fellowship that provides clinical experiences and guides toward professional development.
Fellows Assemble! A Cross-Fellowship Collaborative Approach to Learning
Maureen Welty, DNP, CNP-AC and Amanda Lahood, MSN, FNP-BC
An accredited advanced practice provider fellowship program created opportunities to optimize fellow collaborative learning for shared educational opportunities in clinical, professional, and systems education. The presentation focuses on the varied approaches to achieve this, necessary modifications, and lessons learned.
Using Your Resources: Providing Your Fellows What They Need to Be Successful
Allison Kelly
This presentation describes the resources and tools provided to APP fellows in a pediatric health system to help them know where to turn for personal and professional support. Resources discussed include interdisciplinary personnel presentations used, as well as live/virtual/electronic resources.
Resident/Fellow Showcase – RN Resident EBP/QI/Research Projects — CS-05-L
Stay Ready to Walk Steady! An Evidence-Based Practice Project to Reduce Falls
Corynn Riley and Shavanta Alston
This evidence-based practice project sought to measure the effects of implementation of a unit whiteboard on fall rates in an inpatient setting. The whiteboard was created to be a universal resource to aid in ambulating patients and reducing overall falls.
Artificial Intelligence and Hand Hygiene Monitoring
Braden Damitz, BSN, RN and Russell Ross, BSN, RN
This evidence-based practice project addresses the persistent challenge of hand hygiene non-compliance with Leapfrog standards among all health care professionals and presents a novel approach using Intelligent Observation technology. Acknowledging the gap between recommended infection prevention protocols and practical implementation, the project aims to enhance adherence through electronic hand hygiene monitoring.
Development of a Mock Schedule Template to Assist Newly Licensed Nurses with Time Management
Celine Burns and Owen Kiernan
Increasing Triage Efficiency: The ED Love Language
Ian Harrison, BSN and Emily Swann, BSN
It is highly recognized that the language barrier is a detriment to quality health care. This session describes the creation, application, and results of multiple target language triaging forms for the Emergency Department setting. This form bridges the gap between wait times of interpreter services and expedient patient care.
Noon – 1:00 p.m.
Lunch and Sponsor Tables
12:45 p.m.– 1:45 p.m.
Poster Presenters Available
1:45 p.m.– 3:00 p.m.
General Session 2; GS-02
Celebration
Finding Florence: Keeping Well-Being a Priority Throughout Your Professional Career
Tim Cunningham, DrPH, MSN, RN, FAAN
This interactive keynote presentation brings the audience together through laughter, some thought-provoking activities, and most of all, the recognition that nurses are here to heal. As healers, nurses must know how to keep well-being alive and present in all that they do. Through storytelling, lessons of physics, and a game or two, Cunningham engages the audience in forging ahead on their own well-being journeys.
3:00 p.m. – 3:15 p.m.
Break
Tim Cunningham book signing
3:15 p.m.– 4:15 p.m.
Concurrent Session 6; CS-06
TTP Solution – Well-being — CS-06-A
The First Year in Nursing: Preventing New Nurses from "Snapping Their Caps"
Jocelyn Marx, MSN, RN-BC, HNB-BC and Sara Scheller Humeny, MS, BSN, RN, NBC-HWC, HNB-BC
Nurse well-being goes beyond a requirement of PTAP standards. How do organizations recruit, retain, and support nurses to find balance and grow into role models for promoting wellness in their communities? Using a multi-pronged team approach, nurses are educated and supported in their first year and beyond.
R.I.S.E. – Resident Integration of Supportive Experiences
Sophy Rodriguez, MSN, RN, CPN and Karen Pierce, MSN, PED-BC, CCRN-K, NPD-BC
An innovative immersion experience for nurse residents incorporating coaching and well-being, shadow experiences, and interprofessional simulation scenarios.
Building Resilient Nurses: Integration of Self-Reflective and Well-being Initiatives for New Graduate RNs
Vanessa Lopez, MSN, RN, NPD-BC and Kimberly Hutapea, PhD, MSN, RN
Presenters share implementation of evidence-based strategies to build resilience, enhance wellness, develop clinical nursing judgement within a new graduate RN transition to practice program across a multisite health care system.
TTP Power – APP Curriculum — CS-06-I
Promoting Diversity and Inclusion: An Innovative APP Fellowship Recruitment Strategy
Amelia Cataldo, DNP, RN, CPNP-AC, CCRN and Nicole Zakak, MS, RN, CPNP, CPHON
Diversity and inclusion are important values to promote employee satisfaction and belongingness and to guide recruitment and retention strategies in organizations. This presentation highlights an innovative strategy to promote the recruitment of a diverse APP fellowship class and shares best practices for retention of diverse talent.
Addressing Advanced Practice Resident/Fellow Anxiety with a Cognitive Behavioral Therapy Exercise
Kameren Owens, MSN, FNP-C
The presentation shows prevalence and reviews literature about anxiety among new clinicians. It provides a brief overview of cognitive behavioral therapy (CBT), as well as a walk-through CBT exercise in which the audience can choose to participate. Discussion follows of how this exercise can be used with residents/fellows.
Learner Focused Seminar – DEI and Belonging — CS-06-K
The Power of DEI + Belonging
Suzanne Knight, DNP, RN, NPD-BC and Maria Bobo, DNP, RN, WHNP-BC, CENP, NPD-BC
This engaging and interactive session is based on the fellowship's curriculum that promotes a culture of diversity, equity, inclusion (DEI), and belonging. The session will help learners identify their comfort level in addressing DEI issues, gain tools to address situations related to DEI, and create inclusive teams.
TTP Power – Engaging Faculty and New Grads — CS-06-M
Faculty Evaluation Using the ENGAGE Model
Kim Failla, PhD, RN, NE-BC, NPD-BC and Courtney Kendal, MSN, RN, CNS, NPD-BC
This presentation describes the development and implementation of a tool used by the program director (or designee) to evaluate faculty. The evaluation tool, based on the ENGAGE Model, uses a 4-point Likert scale, has 20 items, and two open-ended questions. Use of the tool can guide faculty enhancements.
Grounding Your "Flight Risks"
Debbie Rimmele, BSN, OCN, CPC and Cheryl Nazal, MS, APRN-CNS, NPD-BC, NE-BC, ACNS-BC
Turnover of new graduate nurses is costly and negatively affects patient care and staff satisfaction. Early identification turnover risk is key to engagement and retention. A standardized approach that defines interventions to retain new nurses demonstrated reduced turnover. The process and interventions can be implemented to retain flight-risk employees.
TTP Power – Nursing Excellence — CS-06-L
Evidence-Based Framework for Creating Positive Practice and Learning Environments
Melissa Bates, DNP, RN, CDE
The National Academy of Medicine’s Action Collaborative on Well-Being and Resilience recently released the National Plan for Health Workforce Well-Being. Seven priority areas were identified and the number one priority is to “Create positive learning and work environments for nurses.” This presentation discusses an evidence-based framework for supporting nurses as they transition to practice.
Finding Our Way Forward: a Roadmap for the Future
Monica Work, MSN, RN, NE-BC
The last few years have been rife with challenges, but it was also a time when nurses were able to demonstrate their innovation and strength. The evidence-based framework of ANCC’s Magnet Recognition Program® provides a structure that promotes nurse engagement and improved patient outcomes. Using shared decision-making, nursing research, evidence-based practice, nurse autonomy, and interprofessional collaboration, organizations can build a shared vision for an even stronger future.
4:15 p.m.– 4:30 p.m.
Break
4:30 p.m.– 5:30 p.m.
Concurrent Session 7; CS-07
CS-07-A
CS-07-I
CS-07-K
CS-07-M
CS-07-L
7:30 a.m. – 8:30 a.m.
Breakfast and Poster Viewing
8:30 a.m.– 9:30 a.m.
Concurrent Session 8; CS-08
TTP Power – Leadership — CS-08-A
Covering All the Bases: Development of Standard Work and RN Coordinator to Resident Ratios
Randy McClain, DNP, RN, NEA-BC and Carrie Davis, MSN-Ed, RN, NPD-BC
Developing an RN Residency team is critical, but how many players does it take to knock outcomes out of the park? Participants will discover how one organization’s system created standard work for RN residency coordinators, and developed recommendations for coordinator-to-resident ratios, facilitating a balanced workload and resident success.
Unlocking the Power of VOICE: Empowering Novice Nurses through Meaningful Connections with Nursing Leaders
Elena Cereceda, MS, BSN, RN, NPD-BC
Discover the VOICE program, an initiative forging connections between executive nursing leaders and novice nurses. This program bridges the gap between organizational and bedside leaders, enhancing empowerment of clinicians, creating opportunities for insightful collaboration, catalyzing change in practice, and fostering a culture of trust and responsiveness.
Strategic Planning Speaking C-Suite for Culture Change
Alaina Tellson, PhD, RN, CLNC, NPD-BC, NE-BC
This presentation discusses strategic planning to drive culture change, understanding how to communicate effectively with the C-suite and alignment to the organization's goals. Included is how to align the strategic plan to the organization's strategic plan, mission, vision, and values to drive program goals and outcomes.
TTP Power – APP Fellowship – Organizational Support — CS-08-I
Maintaining Operational Consistency: Streamlining Communications and Operations across Subspecialty Tracks in a Large APP Fellowship
Amelia Cataldo, DNP, RN, CPNP-AC, CCRN and Linda McKenna, MSN, RN, AGACNP-BC, ANP-BC, CNS-C
Large APP fellowships with multiple subspecialties risk inconsistencies of operations across subspecialties. This presentation highlights best practices to maintain standardization of operations across subspecialties in a large fellowship program including centralized leadership and optimal communication strategies.
Rallying Institutional Support for the Establishment and Maintenance of an Advanced Practice Provider Fellowship
Suzette Stone, PhD, PPCNP-BC, NEA-BC and Tonya Ureda, MS, RN, FNP-BC, NE-BC
Participants will explore operational readiness for launching and maintaining an APP fellowship by engaging stakeholders across the organization.
Learner Focused Seminar – Precepting — CS-08-K
Going for Gold: Become a Champion Preceptor
Dawn P. Bradley, MSN Ed., NPD-BC, CPN and Lauren Frahm, MSN, RN, NPD-BC
Current and former nurse residents will benefit from this workshop that explores best practices for preceptorship through interactive activities, story sharing, and self-reflection. The overall goal is to empower preceptors to lead with confidence and compassion to support the practice transition of new nurses.
TTP Solution – Development and Design — CS-08-M
The Power of Independent Practice: Learner-Focused Approach Identifying Learning Needs and Closing Practice Gaps
Cynthia Crockett, MSN, RN, NPD-BC and Erika Wollitzer
This presentation highlights the development and design of using the concept of independent practice to identify nurse residents’ unique learning needs and address practice gaps. The data presented will show the power of independent practice, reflecting on individualized learning needs, and building nurse residents’ confidence and competence.
Building the Case! Utilizing Case Presentations to Enhance Competence in Evidence- Based Practice
Melanie Mudd, MS, RN, NPD-BC
Many nurse residency programs utilize evidence-based practice (EBP) projects to improve patient outcomes, as well as foster clinical reasoning and critical thinking. This session provides an innovative alternative to giving new graduate nurses the opportunity to apply EBP principles within a health care organization.
Building Bridges to Success: Connecting ANA Scope and Standards of Practice into PTAP Residency
Angelica Acosta and Amy Hartnett
This organization utilizes a "Daily Orientation Progress Evaluation" tool, which integrates ANA's Scope and Standards of Practice into daily goal setting and reflection. This practice allows the scope and standards to be introduced to the new graduate nurse and emphasized by the preceptor with context as they go through training.
TTP Power Session — CS-08-L
Humanness in Learning
Jennifer Graebe MSN, RN, NEA-BC
Humanness in learning complements intellectual behaviors by infusing them with empathy, collaboration, and emotional depth. It fosters critical thinking, creativity, and ethical values, enriching the educational journey. Focusing on humanness in the learning environment enhances comprehension, motivation, and the development of well-rounded individuals who are not only intellectually adept but also socially and emotionally aware.
9:30 a.m.– 9:45 a.m.
Break
9:45 a.m.– 10:45 a.m.
Concurrent Session 9; CS-09
TTP Solution – Well-being — CS-09-A
Principles of Recovery
Simmy King, DNP, MS, MBA, RN-BC, NE-BC, CHSE, FAAN and Kristi Myers, MSN, RN, CPN
This presentation describes how nurses experience stress and provides strategies on how to recover from stress. In addition, participants will learn the difference between stress response and stress recovery and how an individual’s personal ecosystem impacts how they experience stress.
Activating a Second Line of Support: Caring for Our Newest Caregivers
Patricia Marie Sarver, DNP, MSN, RN, NE-BC, CNE, NPD-BC, CPN
This presentation identifies how one organization implemented a unique way to demonstrate care for its nurse residents and provide them an ongoing opportunity throughout their first year of practice to discuss concerns, realize they are not alone, and minimize stress.
Enculturating Calm: A Layered Approach to Promote Resiliency in Transition to Practice
Kerry Zoss, MS, RN, NPD-BC, PCCN-K and Kristi Norris, MSN, RN, NPD-BC, CMSRN
Participants will explore a well-being program that fosters peer support, decreases feelings of isolation, and promotes self-compassion and wellness by utilizing a three-part lecture series focused on self-care and stress management, facilitator-led small group reflection sessions, peer support opportunities, journal exercises, seminar session pulse checks, and leader-driven progression debriefs.
TTP Power – Preceptors – APP Fellowship — CS-09-I
Establishing and Designing a Standardized Preceptor Class for Advanced Practice Provider Transition to Practice Program
Courtney Coker, MSN, RN, AGACNP-BC and Will Westmoreland, MSN, RN, AGACNP-BC
Establishing a standardized preceptor class for individuals responsible for teaching and mentoring new advanced practice providers is a critical initiative with many benefits such as consistency in didactic information, standardization of expectations of new learners, and education regarding providing constructive feedback.
Benefits of a Structured Preceptorship Program and the Value of the Preceptor Ambassador
Evelyn P Wempe, DNP, MBA, APRN, ACNP-BC, AOCNP, NE-BC
Presenters describe the structure and impact of a preceptorship program as part of an APP fellowship and the role of the preceptor ambassador in recruitment, onboarding, education, and support of advanced practice preceptors.
Learner Focused Seminar — CS-09-K
Jazz Up Your Passion for the ANA Code of Ethics
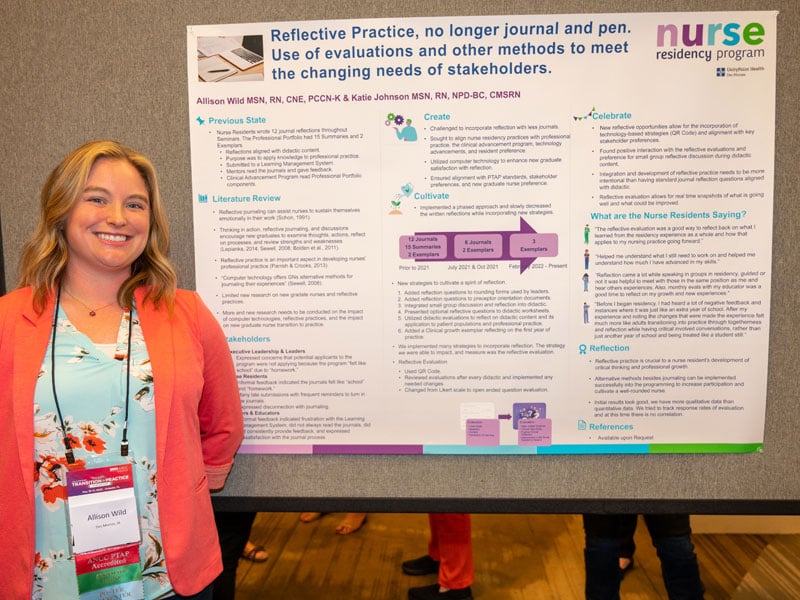
Katie Johnson, MSN, RN, NPD-BC, CMSRN and Allison Wild, MSN, RN, CNE, PCCN-K
Educators align teaching and learning strategies to engage the learner. This presentation shares how one hospital found the melody of the ANA Code of Ethics by getting back to the basics of adult learning and using the teach-back method to bridge the gap from words on paper to application to practice.
TTP Power – Communication — CS-09-M
BERT Nursing Simulation – A Live-Action Experience
Debra Rodgers, MSN, RN, CNL and Sheryl Rickord, BSN, RN, CHSE, CHSOS
The presentation describes the design, objectives, and implications to nursing practice of new graduate nurses for the interdisciplinary behavioral emergency nursing simulation conducted within the nurse residency program on recognizing and acting on escalating behaviors within patient care to call a Behavioral Emergency Response Team (BERT) alert.
Applying Communication Strategies in a Psychologically Safe Environment
Lauren Danforth, MSN, RN, NPD-BC
Nurse residents (NR) are challenged with communication in the clinical environment, specifically communicating with providers and families. A simulated experience with small groups rotations allowed for NRs to practice communication skills in a psychologically safe environment.
TTP Power – Advancing TTP Research — CS-09-L
Bridging the Gap: Integrating Nursing Transition to Practice with Research
Marcela Cámpoli, PhD, MHA, BA, ASQ CQM/OE
The intersection between nursing transition to practice and research/EBP/QI/Innovation is pivotal in health care. This presentation underscores the integration of research/EBP/QI/Innovation during the onboarding of novice nurses, emphasizing mentorship and structured programs to foster a culture of inquiry. By nurturing research/EBP/QI/Innovation, health care institutions empower new nurses to contribute effectively in an ever-evolving health care landscape
10:45 a.m.– 11:00 a.m.
Beth Ulrich book signing
11:15 a.m. – 12:30 p.m.
General Session 3; GS-03
Closing Remarks
Mastering Precepting to Ensure the Success of the Next Generation of Nurses
Beth Ulrich, EdD, RN, FACHE, FAONL, FAAN
Preceptors live at the intersection of the present and the future. They are the essential link between what nurses are taught and what they do, and between what they know and what they need to know. In this closing general session, the audience will learn practical ways to ensure that preceptors are successful.
PS-01 - Personalizing and Creating a Culture of Wellness with AACN’s Healthy Work Environment Framework
Elena Fontan, RN
This presentation describes a transformative approach to creating a culture of wellness with the AACN Healthy Work Environment (HWE) six standards framework. Participants will dive into nursing-specific interventions aligned with AACN's standards, enhancing communication, collaboration, decision-making, staffing, recognition, and leadership. They will learn how this comprehensive approach empowers nurses, cultivates well-being, and elevates patient care.
PS-02 - Decreasing Catheter-Associated Urinary Tract Infections (CAUTI) in Surgical Oncology Patients
Elaine Hawe, BSN, RN
The daily safety huddle sheet was edited to add a red and green sticker section to increase nurse awareness of each patient's need for an indwelling urinary catheter. The goal of this evidence-based practice project was to decrease CAUTIs.
PS-03 - Preventing ED Workplace Violence in the Emergency Department Using an Inclusive Approach
Julia Ewen, BSN, RN and Jenna Castilletti, BSN, RN
The primary goal was to decrease workplace violence (WPV) in the ED through the use of evidence-based strategies within an inclusive workplace framework to design, implement, and sustain an effective department-wide WPV preventive bundle. This evidenced-based project is in the implementation phase of the residency project started last year.
PS-04 - Prevention of Post-Operative Delirium in Oncology Patients
Nicole Bespalov, BSN, CCRN
Post-operative delirium leads to longer lengths of stay, higher rates of falls, more pain, and functional decline in older patients. Post-operative delirium prevalence (POD) was tracked by results of the Confusion Assessment Method (CAM), and a POD bundle was implemented in the ICU and surgical step down units.
PS-05 - Red Lights on Nights
Kendra Deschamps and Kathleen Caporelli, MSN, RN, MEDSURG-BC, CHPN
Implementing a red light clip system compared to a white-light system for RNs and PCAs to wear improved patient sleep quality and patient satisfaction.
PS-06 - Structuring a Subspecialty Fellowship Track in Geriatric Oncology
Sincere McMillan, DNP, MS, RN, ANP-BC
This presentation highlights the development and implementation of a geriatric oncology subspecialty fellowship track. Geriatric oncology is a subspecialty of medicine focusing on the care of older adults with cancer. After viewing this poster, participants will be able to describe the current track structure and goals.
PS-07 - Enhancing Professional Development and Transition to Practice in an APP Oncology Fellowship through Specialized Education
Sarah Rebal, ACNP-BC and Linda McKenna, AGACNP-BC, ANP-BC, CCRN-CMC
Didactic content is essential for a well-rounded APP fellowship curriculum. The APP oncology fellowship described in this presentation is comprised of 10 subspecialty tracks, each with unique learning objectives. This presentation describes the challenges faced and barriers overcome in creating a didactic learning curriculum that united all subspecialties.
PS-08 - Transitioning APPs to a Highly Specialized Practice: The Role of a Neuro-Oncology APP Fellowship Program
Linda McKenna, AGACNP-BC, ANP-BC, CCRN-CMC and Amelia Cataldo, DNP, PNP-BC
The American Academy of Neurology supports the integration of APPs to improve access to high-quality neurological care, but formal graduate education for APPs does not include training in this specialty. This poster describes the impact a neuro-oncology APP fellowship program has on the APP's transition to independent neurology practice.
PS-09 - Reflective Conversations Facilitation Using the Reflect Tool: Conversation Prompts for Transitional Experiences
Mykell Barnacle, FNP/DNP and Deb Steen, MSN, APRN, CNP
Many transition to practice programs require reflective journaling to solidify learning and promote professional growth, self-awareness, and clinical competency. However, requiring written reflections can be onerous for adult learners. Reflective conversations in a rural NP residency program balance the importance of reflection with the learning style best suited to graduate NPs.
PS-10 - Promoting Professional Development Like a Pro for Nurses Participating in Practice Transition Programs
Beth Cook, MSN, RN, CNL, NPD-BC, CHSE, CCRN-CSC and Shannon Beck
Promoting professional development is a quality outcome measure for this organization’s critical care fellowship program. Tips and tricks are shared to promote engagement in professional development, including participating in local professional organizations for nurse residents or fellows.
PS-11 - Home (Care) Wasn't Built in a Day: Our Nurse Residency Program Journey
Nancy Linscheid, MSN, RN, COS-C and Jennifer Delagardelle, MSN, RN
Participants will explore the development of a nurse residency program that meets the needs of newly licensed registered nurses in the specialties of home care and hospice.
PS-12 - Tracking Nurse Resident Stress Levels Coupled with Targeted Interventions
Gail Cudia, MSN, BS, PED-BC and Danielle Hilliard, MSN, APN, CPNP, NPD-BC, CCRN-K
In an effort to help program faculty identify nurse residents struggling with stress and support their well-being, the "Perceived Stress Scale" was introduced into this facility's residency program. The tracking of these scores throughout each nurse's residency enables program faculty to identify residents struggling with stress, and intervene early.
PS-13 - Stakeholder Evaluation Survey for Nurse Fellowship Programs
Kim Failla, PhD, RN, NE-BC, NPD-BC and Laurie Ecoff, PhD, RN, NEA-BC, CNL
This presentation describes how a stakeholder evaluation survey was revised to be used by nurse fellowship programs. The instrument uses a 4-point Likert scale and has 43 items. Use of the psychometrically validated instrument can guide fellowship program enhancements and outcomes.
PS-14 - After the Residency: Engaging Nurses with a Peer Advisor Program
Michelle Cook, MS, RN, NPD-BC, CHPPN and Pamela Gehrich, MSN, RN, NPD-BC, CPN
One organization's innovative way to engage recent RN residency graduates was through a Peer Advisor Program. Details of the program's design, along with benefits for both the peer advisors and new RN residents are shared.
PS-15 - Artificial Intelligence in Nursing Transition Practice Programs
Hanan Alfahd, PhD, MME, RN
The integration of AI in nursing education and clinical settings, including practice transition programs, needs collaborative reform from nursing organizations to prepare nurses to practice safely and competently in the era of AI.


PS-16 - Resident Professional Advancement and Learning Support (rPALS): Peer Mentoring within the Nurse Resident Program
Leilanie Gacayan Apana, MSN, RN, NPD-BC
New graduate nurse residents (NGNR) identified the need for constant peer-to-peer support and collaborative relationships with colleagues who "knew what they were going through." Former NGNRs were amicable to offer emotional corroboration and share lived experiences with current NGNRs in the nurse residency program.
PS-17 - Remembering Our Why: Keeping Learner Engagement a Priority
Brandi Sieminski, BSN, RN, NPD-BC, CMSRN and Charity Ballmann, MSN, BA, RN, CNML, MEDSURG-BC, NEA-BC
This presentation features strategic tactics to engage nurse resident learners, thus contributing to the overall success of an organization’s nurse residency program.
PS-18 - Empowering Early-Career Nurses to Advocacy and Civic Engagement
Lya M. Cartwright-Stroupe and Eric Small
Professional advocacy is a critical dimension for the sustainability of the nursing profession. Early-career professional programs create an opportunity to elevate the voice of nursing by engaging in advocacy and civic engagement. This session describes a study of early-career nurses and avenues of advocacy.
PS-19 - The Carousel of Knowledge: Our Approach to an Open Enrollment Nurse Residency Program
Deborah Baldassarre, MSN, RN, OCN, NPD-BC and Diana Kott, MSN, RN, OCN, NPD-BC
This presentation shows how the nurse residency coordinator and nursing professional development team met the nursing shortage and clinical skills development needs by opening nurse residency enrollment and extending skills training. The program allows nurse residents to onboard at any time and receive crucial education, no matter where they hop on the carousel.
PS-20 - Organize Residents' Learning Experience Based on Knowledge, Skills, and Attitudes
Eman M. Othman, MSN, RN
This presentation shares a best practice of the nursing education team in implementing the nursing residency program by utilizing a color-coded workbook that organizes learning based on knowledge, skills, and attitudes.